Recovery Isn’t One-Size-Fits-All
Medication-assisted treatment (MAT) is a proven tool in the fight against addiction. It helps reduce cravings, stabilize mood, and prevent relapse. But for some patients, progress feels out of reach despite following every recommendation.
We’ve seen this firsthand at BloomDNA. Some people respond quickly to MAT. Others struggle with side effects or feel no benefit at all. This gap often comes down to something that hasn’t been part of the traditional process: your DNA.
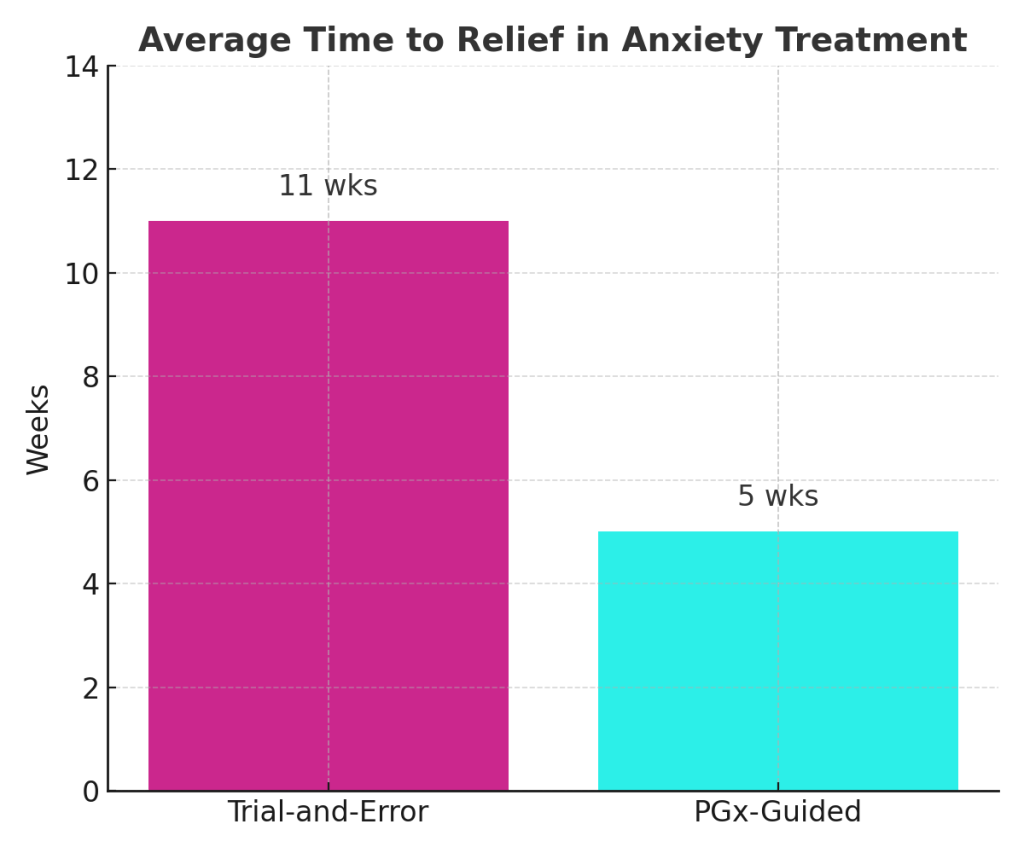
Pharmacogenetic (PGx) testing helps identify how your body processes specific medications, offering providers a clearer roadmap for care. For patients like Marcus, it changed everything.
Source: Muriel J. et al. (2023). Impact of CYP2D6 genotype on opioid use disorder tapering outcomes.
🔗 Frontiers in Pharmacology
A Patient Story That Changed Direction
Marcus had relapsed after two inpatient stays. MAT was part of his plan, and he followed it closely. But after a few weeks, cravings returned. His energy dropped. His motivation disappeared.
His provider adjusted the dose. Switched medications. Added behavioral support. Nothing seemed to work long-term.
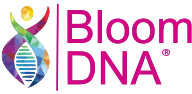
They turned to BloomDNA® for a pharmacogenetic test. The results showed Marcus had reduced CYP2D6 enzyme activity, meaning his body couldn’t effectively process his medication. Based on this insight, his provider adjusted his prescription again—this time in line with his metabolism. Within weeks, Marcus reported fewer cravings and more stable focus throughout the day.
Source: Muriel J. et al. (2023). Impact of CYP2D6 genotype on opioid use disorder tapering outcomes.
🔗 Frontiers in Pharmacology
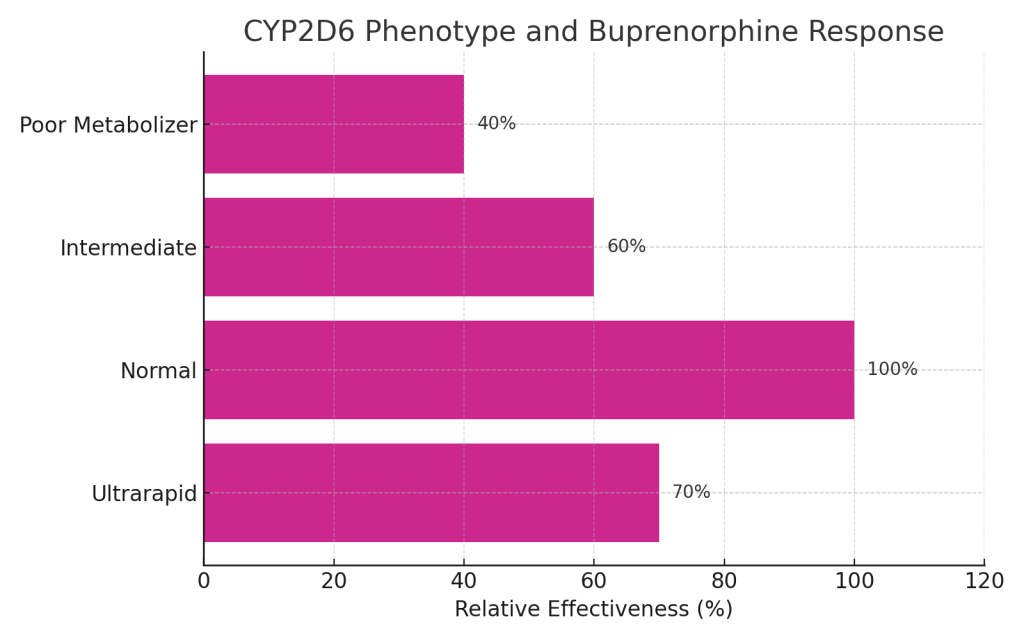
What PGx Testing Does in Addiction Treatment
Pharmacogenetics studies how your genes influence your response to medications. For addiction care, it can explain why one MAT protocol works well for one patient and not for another.
It’s especially helpful for medications like:
These drugs interact with opioid receptors in the brain and are metabolized through various genetic pathways. When those pathways are impaired or overactive, the expected results may not occur—or may come with complications.
- Buprenorphine
- Naltrexone
- Methadone
Source: Kusic D. et al. (2022). Patient perceptions of pharmacogenetic testing in chronic pain and OUD.
🔗 MDPI Pharmaceutics
Key Genes We Analyze
BloomDNA’s clinical-grade test reviews several gene markers known to impact MAT outcomes:
- CYP2D6 and CYP3A4 – Influence how your liver processes many addiction medications
- OPRM1 – Impacts how opioid receptors respond to medications like naltrexone
- COMT and DRD2 – Affect dopamine activity, which plays a role in reward response and motivation
Your provider receives a personalized report that explains which medications may be more compatible and what to monitor for when choosing or adjusting treatment.
Provider Perspective: Why This Matters in Clinical Practice
“In addiction care, timing and clarity matter. When we start with pharmacogenetic insight, we avoid unnecessary delays and reduce patient frustration. It doesn’t replace clinical judgment—it supports it.”
— Dr. Carla Mendez, Addiction Medicine Specialist
Source: Reynolds KK et al. (2008). CYP2D6 and OPRM1 pharmacogenetic testing regarding opioid treatment.
🔗 PubMed
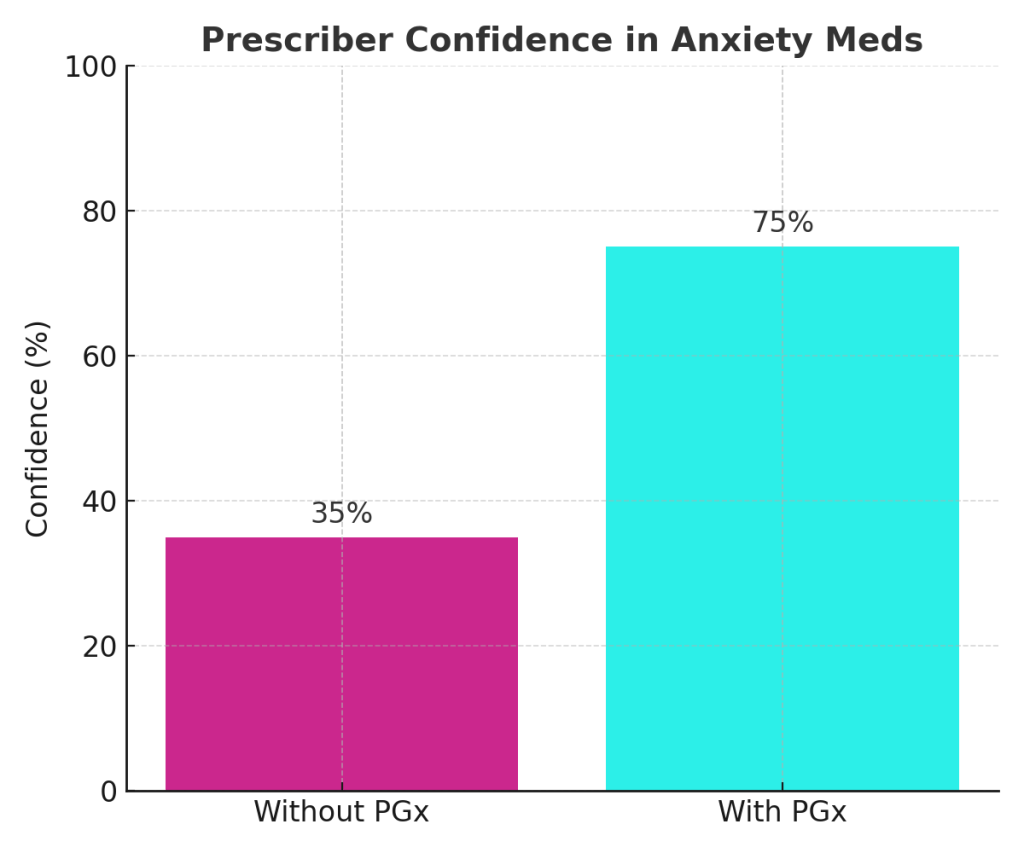
Providers often work with patients who have tried multiple medications without long-term success. PGx testing helps them quickly identify which treatment paths are more likely to produce results. It also helps explain why past treatments failed, which is essential for patient trust.
Having this information at the beginning of MAT planning allows for better decisions, stronger adherence, and fewer avoidable side effects.
Why Choose BloomDNA for PGx Testing
Our reports are built for providers and written with patients in mind. Every BloomDNA® test includes:
- Clinical-grade analysis of over 300 medications
- Focused results for addiction, mental health, and physical health
- A patient-friendly report that providers can reference directly
- Processing by a certified U.S.-based lab with strict quality review
This test can serve as a lifelong guide for medication planning and help eliminate unnecessary risk during recovery.
Take the Next Step With More Certainty
If you’ve started MAT and it doesn’t feel right, or you’re about to begin, pharmacogenetic testing can provide answers your provider needs to make more confident decisions.
Explore how pharmacogenetics can work for your condition.
References
Seguí HA
et al., A review of the pharmacogenomics of buprenorphine for opioid use disorder — This review covers pharmacogenomic data in the context of MAT with buprenorphine.
https://www.oaepublish.com/articles/jtgg.2020.35 oaepublish.com
Muriel J
et al., Impact of CYP2D6 genotype on opioid use disorder tapering outcomes — Observational study showing how CYP2D6 phenotypes affect OUD treatment and withdrawal outcomes.
https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2023.1200430/full%20Frontiers
Kusic D
et al., Patient Perceptions and Potential Utility of Pharmacogenetic Testing in Chronic Pain Management and Opioid Use Disorder (Camden Opioid Research Initiative) — Shows patient openness to PGx in chronic pain and OUD contexts.
https://www.mdpi.com/1999-4923/14/9/1863 MDPI
David V
et al., An Analysis of Pharmacogenomic‑Guided Pathways and Hospitalization Outcomes — Demonstrates broader evidence for PGx‑guided medication changes and reduced hospitalization, relevant to addiction pharmacotherapy.
https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2021.698148/full Frontiers
Reynolds KK
et al., The Value of CYP2D6 and OPRM1 Pharmacogenetic Testing Regarding Opioid Treatment — Explores how these genetic markers influence opioid use, efficacy and addiction risk.
https://pubmed.ncbi.nlm.nih.gov/19059064/ pubmed.ncbi.nlm.nih.gov
Sources
- Muriel J. et al., Frontiers in Pharmacology (2023): CYP2D6 & OUD Tapering Outcomes
- David V. et al., Frontiers in Genetics (2021): PGx Pathways and Hospitalization Outcomes
- Kusic D. et al., Pharmaceutics (2022): PGx Perceptions in OUD Care
- Reynolds KK. et al., PubMed (2008): OPRM1 and Opioid Treatment