Why More Doctors Are Turning to Pharmacogenetic Testing
Your DNA may hold the key to safer, more effective medication choices
When a doctor prescribes a medication, there’s usually one big assumption: that it will work for you. But for millions of people, that first prescription leads to unexpected side effects or no relief at all. This trial-and-error approach to treatment can be frustrating, expensive, and even dangerous. That’s why more healthcare providers are turning to a powerful tool called pharmacogenetic testing — also known as PGx testing.
PGx testing helps doctors understand how your genetic makeup affects the way your body processes medications. It’s part of a growing movement toward personalized medicine, where treatment decisions are tailored to the individual instead of using a one-size-fits-all approach.
Let’s break down why this matters, and how it could change your next trip to the pharmacy.
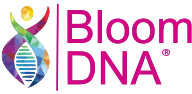
Why First Medications Often Fail — And How PGx Helps
- First medication failure rate drops from 50% to 25% with PGx
- Side effect risk reduced by 67%
- Time to relief shortens from 8 to 3 weeks
- Prescriber confidence more than doubles
What Is Pharmacogenetic (PGx) Testing?
Pharmacogenetics is the study of how your genes affect your body’s response to medications. Your DNA can influence how quickly or slowly you metabolize drugs, how sensitive you are to them, and whether a specific medication is likely to work or cause harmful side effects.
PGx testing typically analyzes key genes like:
- CYP2D6 and CYP2C19, which affect how antidepressants, opioids, and beta-blockers are broken down
- SLC6A4, involved in serotonin transport and response to SSRIs
- VKORC1 and CYP2C9, which influence how you process blood thinners like warfarin
When these genes vary from person to person — and they often do — medications may behave differently in your body than expected.
Why Traditional Prescribing Often Misses the Mark
Doctors have long relied on population averages when prescribing medications. These averages are based on clinical trials that don’t fully account for individual genetic differences. So what works well for one patient might not work at all for another.
According to the FDA, over 250 medications now include pharmacogenetic information on their labels. These include drugs for:
- Mental health (antidepressants, antipsychotics, anxiety medications)
- Pain management (opioids, NSAIDs)
- Heart conditions (beta-blockers, anticoagulants, statins)
- Cancer treatments (chemotherapy agents)
Yet most people still aren’t tested before being prescribed them.
What PGx Testing Reveals
A PGx test looks for variations in your genes that can affect drug response. The results provide:
- A list of medications that may not work well for you
- Medications that could cause serious side effects based on your genetics
- Safer alternatives or recommended dosage adjustments
- Insights your doctor can use to guide treatment more effectively
The test is done once, but the insights last a lifetime. Your DNA doesn’t change, so the results can be referenced again and again as your health needs evolve.
PGx vs. Trial and Error: A Clear Advantage
Here’s an example: Two people are prescribed the same antidepressant. One sees improvement in two weeks. The other feels worse — experiencing fatigue, nausea, or even worsening anxiety. The difference? One person may be a poor metabolizer of that drug due to a CYP2C19 gene variant.
With PGx testing, doctors can identify these variations ahead of time and adjust the prescription to avoid those issues altogether.
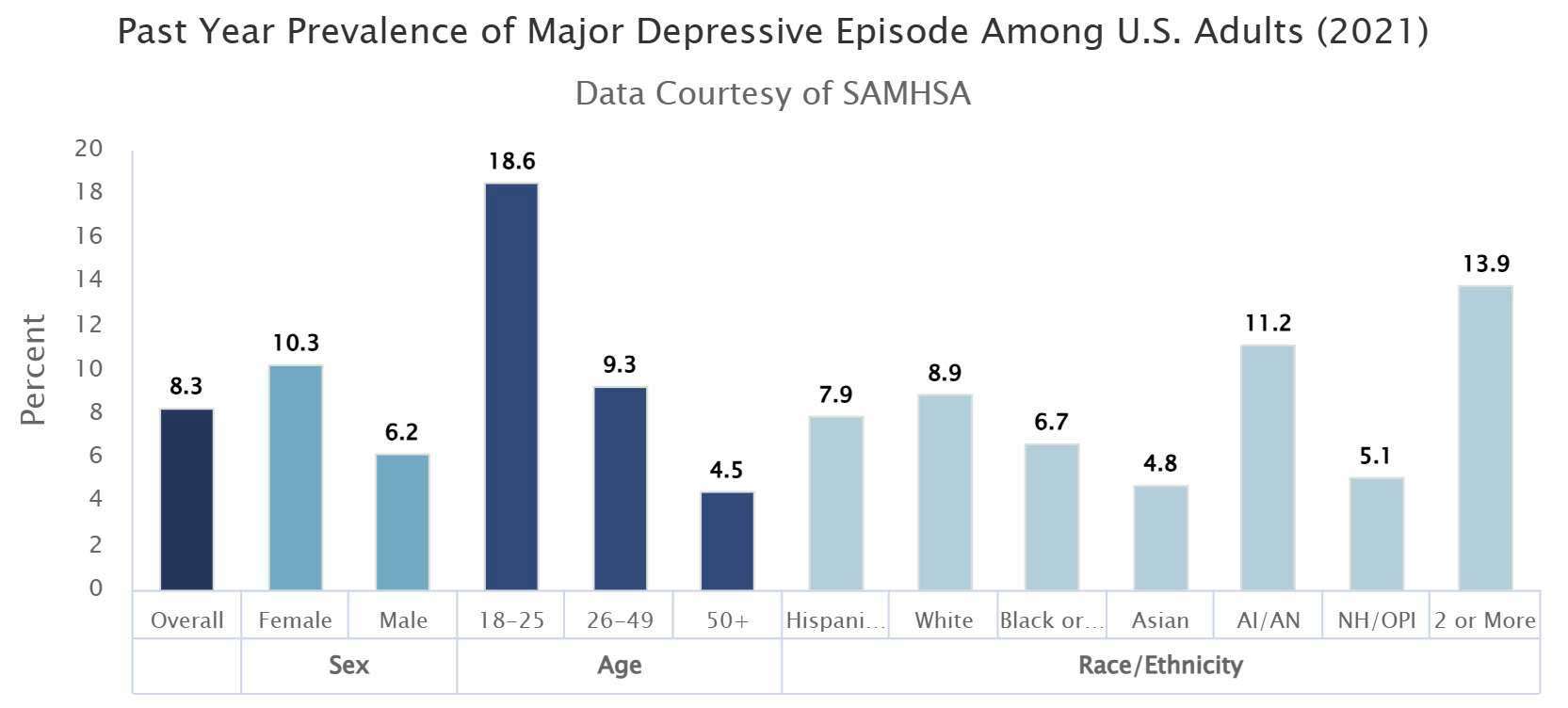
*Persons of Hispanic origin may be of any race; all other racial/ethnic groups are non-Hispanic | AI/AN = American Indian / Alaskan Native | NH/OPI = Native Hawaiian / Other Pacific Islander.
📊 Up to 50% of patients don’t respond to their first prescribed medication for conditions like anxiety or depression.
Source: National Institute of Mental Health
Real Impact: How PGx Improves Care
Studies show that PGx-guided prescribing can reduce:
- Medication trial cycles by identifying likely non-responders
- Hospital visits related to adverse drug reactions
- Side effects that lead to patient non-compliance
- Delays in care when initial treatments fail
It’s not just about improving comfort — it’s about safety, speed, and cost. With more insurers recognizing the value of PGx, some tests are now covered or reimbursed under certain plans.
Who Should Consider PGx Testing?
Pharmacogenetic testing may be helpful for:
- Anyone taking multiple medications
- People who have experienced side effects or poor results from common treatments
- Individuals managing chronic conditions like depression, ADHD, anxiety, heart disease, or chronic pain
- Patients considering new long-term medications
- Those with a family history of medication sensitivity
How BloomDNA® Makes Testing Simple
At BloomDNA®, our clinical-grade PGx test is designed for real-world healthcare use. Here’s how it works:
- You order your kit and collect a simple cheek swab at home
- Return it using our prepaid packaging
- Our certified U.S. lab analyzes your DNA
- A licensed provider reviews and delivers your personalized medication report
Your report covers 300+ medications, across key therapeutic areas, with guidance for both patients and their prescribing doctors.
Personalized Medicine Starts Here
In a world where treatment shouldn’t be guesswork, PGx testing provides answers. You don’t have to suffer through ineffective prescriptions, unsafe side effects, or delayed results.
See how your genes could affect your treatment—get tested today.
References
Luzum JA
et al. Moving Pharmacogenetics into Practice: It’s All About the Evidence.
https://www.ncbi.nlm.nih.gov/articles/PMC8376790/
A review summarizing the types of evidence needed for PGx implementation in clinical settings.
Krebs K & Milani L.
Translating pharmacogenomics into clinical decisions: do not let the perfect be the enemy of the good.
https://humgenomics.biomedcentral.com/articles/10.1186/s40246-019-0229-z
Explores barriers and solutions for PGx adoption by clinicians.
Frigon MP
et al. Pharmacogenetic Testing in Primary Care Practice.
https://www.tandfonline.com/doi/full/10.1080/17512433.2019.1635950
Discusses how primary care physicians and pharmacists view PGx testing.
Allen JD
et al. A Scoping Review of Attitudes and Experiences with Pharmacogenomic (PGx) Testing.
https://www.mdpi.com/2075-4426/12/3/425
Highlights patient and provider perceptions of PGx testing and adoption factors.
Saadullah Khani N
et al. A systematic review of pharmacogenetic testing to guide antipsychotic treatment.
https://www.nature.com/articles/s44220-024-00240-2
A recent systematic review showing PGx testing’s potential to improve prescribing and reduce adverse drug reactions.
“Pharmacogenomics for Improved Outcomes and Decreased Costs in Health Care.” American Journal of Managed Care.
https://www.ajmc.com/view/pharmacogenomics-for-improved-outcomes-and-decreased-costs-in-health-care
Shows data on how PGx-guided prescribing can reduce hospitalizations, emergency visits, and cost burdens.